Your Next Colonoscopy Could Get an Assist From AI
Nov. 11, 2022 – Artificial intelligence holds a lot of potential in medicine, helping doctors find skin cancer, flagging potential issues on a chest X-ray, and assisting in many other procedures. Screening for colorectal cancer during a colonoscopy is another prime example.
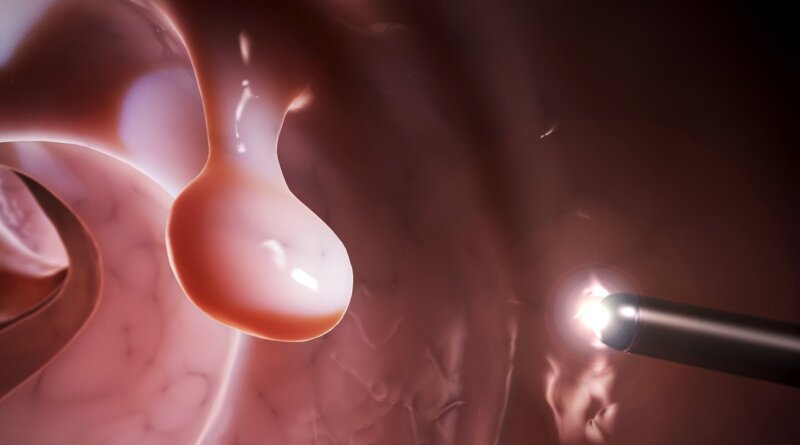
A colonoscopy — recommended for Americans at average cancer risk starting at age 45 — won’t be much different for patients with the addition of artificial intelligence, or AI. But behind the scenes, AI could be making detection of any precancerous polyps or cancerous lesions more likely.
“AI-enhanced colonoscopy effectively turbocharges the physician’s ability to find even the most subtle precancerous polyps,” says Tyler M. Berzin, MD, a gastroenterologist at the Center for Advanced Endoscopy at Beth Israel Deaconess Medical Center in Boston.
The technology is designed to flag anything the computer “sees” as suspicious, but it does not replace the training and expertise of a gastroenterologist. Even with AI, doctors remain at the patient’s side and perform the procedure.
The doctor remains in full control, says Prateek Sharma, MD, a gastroenterologist and professor of medicine at University of Kansas School of Medicine in Kansas City, KS. “AI is assisting and alerting them to colon polyps — the precancerous lesions in the colon — so that the doctor can remove them.”
Controversy Continues
Size, height, and numbers matter with polyps. Doctors generally remove or biopsy lesions 10 millimeters and larger.
But there remains less consensus about the best approach to smaller polyps.
“The clinical relevance of detecting and removing small (5 to 9 mm) or diminutive (less than 5 mm) adenomas is a subject of ongoing debate,” Berzin and co-authors wrote in a leading gastroenterology journal in May 2020.
One of the potential disadvantages to using AI polyp tools, for example, is “the risk of removing a higher number of diminutive or hyperplastic polyps, which increases cost and risk, without any benefit to the patient,” Berzin says.
“Trained gastroenterologists are experts at identifying and removing precancerous colon polyps,” Berzin says. “But a gastroenterologist working with an AI polyp detection tool has a big advantage because AI computer vision tools can simultaneously analyze every pixel of the endoscopy monitor and can do so without being distracted or fatigued for even a millisecond.”
The benefit for patients is “another pair of eyes looking for polyps and helping the doctor,” says Sharma, who is also chair of the Artificial Intelligence Task Force at the American Society for Gastrointestinal Endoscopy.
How It Works
AI is based on computer instructions called algorithms that learn the difference between worrisome and benign colonoscopy images and videos. AI gets better over item in a process called machine learning. When an AI system spots a potential area of concern, the technology calls attention to it by framing it within a box on the screen. Some systems also sound an audible alarm.
“We are seeing more interest in using these algorithms since they will standardize endoscopists’ polyp detection and, therefore, reduce the number of colon cancers missed,” says Sravanthi Parasa, MD, a gastroenterologist at the Swedish Health Services in Seattle.
“These products are slowly gaining traction. During colonoscopy scheduling, patients should ask if their endoscopist has access to augmented diagnostic tools,” she says.
The technology is not accurate 100% of the time – there can be false positives where the system flags a bubble in the colon, for example, as potentially dangerous. That’s just one reason that doctors still have the final say on whether a polyp is suspicious or not.
AI or no AI, “colonoscopy has long been our most effective tool for preventing colon cancer, detecting precancerous polyps earlier than any other screening method,” says Berzin, who is also an associate professor of medicine at Harvard Medical School.
AI Can Be Costly
AI and machine learning already play a role in “smart” technologies (smartphones, smartwatches, and smart speakers), self-driving cars, and speech recognition software. But the use of AI in medicine is comparatively new. And like a lot of novel technologies, it’s also expensive. “The AI equipment needs to be purchased and is expensive,” Sharma says.
“The cost of the algorithms currently can be prohibitive for some centers in the current health care landscape,” Parasa agrees. “The cost is likely to come down as more algorithms enter the GI market, as it is with other software solutions.”
Colorectal Cancer Is Common
Not counting some kinds of skin cancer, colorectal cancer is the fourth most common cancer in Americans. It is also the fourth leading cause of cancer-related deaths in the United States, the CDC reports. More than 150,000 Americans will be diagnosed with colorectal cancer and more than 50,000 will die in 2022, according to National Cancer Institute figures.
Future Insights
More research is needed to examine how humans and this technology interact, Berzin says. “The most interesting research in this space will not be about comparing ‘physician versus AI,’ but will be focused on understanding the nuances of ‘physician plus AI.’”
In the U.S., there are at least three FDA-approved AI algorithms for polyp detection, and more are being developed, Parasa says.
“In addition, other applications which are currently available on the European market might be available in the U.S. market in the near future, including polyp characterization.”
“As the field matures, we will likely see more AI augmentation tools that will assist us in detecting and diagnosing GI conditions in real time,” she adds. “A suite of algorithms like this will definitely improve patient care and outcomes.”
Even though AI is somewhat of a work in progress in medicine, Berzin expects the combination of doctor and AI technology “will translate into the highest possible protection from colon cancer in the long term.”