How Scientists Predict How Many People Will Get COVID-19
What your doctor is reading on Medscape.com:
APRIL 01, 2020 — Projections of the number of people the novel coronavirus could infect, and how many it may ultimately kill, change by the day.
On Tuesday, Deborah Birx, MD, the coronavirus response coordinator for the White House, warned some 100,000 to 240,000 people in the US are likely to die from COVID-19. A little more than a week earlier, on March 21, New York Gov. Andrew Cuomo said he expected between 40% to 80% of New Yorkers to become infected with the new coronavirus, SARS-CoV-2. California’s governor Gavin Newsom landed on the virus reaching 56% of his state in a letter he wrote to President Trump on March 18. And in a study published March 16, researchers from the Imperial College of London cautioned that without adopting social distancing measures, 81% of the US would be infected.
So, what should we expect?
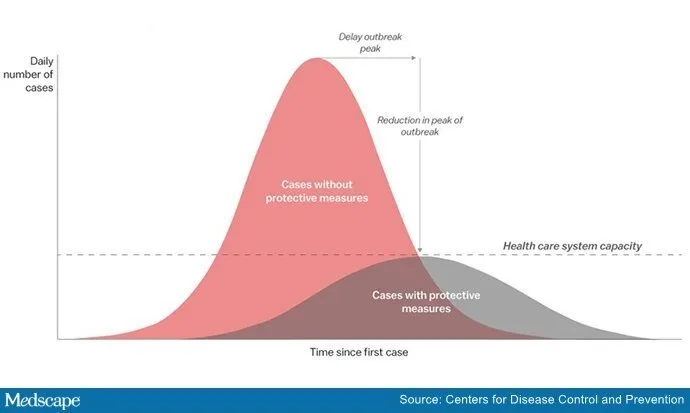
For the general public, these ranges help demonstrate the potential impact of adhering to physical distancing guidelines to substantially reduce the number of infections and stem the flow of patients overwhelming healthcare facilities all at once. Hospital systems and policymakers use these estimates from federal and local levels to anticipate how high the surge of COVID-19 patients might be, and to prepare the intensive care unit beds, emergency room capacity, and ventilators necessary to care for the sick. The Institute for Health Metrics and Evaluation at the University of Washington posts daily updates to its models of future need for hospital resources, and as of Tuesday projected COVID-19 patients will need 220,643 total hospital beds (32,976 in ICUs), and 26,381 ventilators at the epidemic peak on April 15.
Here’s a guide to where these numbers come from.
To model the course of an epidemic, epidemiologists need to know how contagious a virus is, how long people are infectious, the number of people currently infected, and the population susceptible to infection. Models can also account for basic characteristics of a community such as population density, age distribution, underlying health, average household size, and the frequency and nature of social interactions.
Continued
The predictions typically include ranges from a best-case-scenario to the worst. Some variables change based on dynamics of individual communities, and others depend on the effectiveness of stay-at-home orders. Another source of variability between different models is a result of working in the early days of this virus, just 4 months old in humans. “This is totally new,” says Henry Raymond, DrPh, MPH, an epidemiologist at Rutgers University School of Public Health in New Jersey. “It has its own characteristics that make comparing it or using data from other outbreaks just estimations.”
What Scientists Seem to Know
One basic, vital point that feeds into these models is, on average, how many people one infected person will spread the virus to, known as “R naught (R0).” Without efforts to contain the virus, that number is somewhere around 2.4, according to researchers at the Imperial College of London, and scientists place its lower and upper bounds near 2 and 3, respectively. This is more contagious than the seasonal flu, which has an average R0 of 1.3, but not as transmissible as chickenpox (R0 of over 10) or measles (R0 over 12).
“That parameter shapes the epidemic in critical ways — how quickly we accelerate in the exponential phase, how quickly we reach a peak, how high it is, and then its descent,” says Yonatan Grad, MD, PhD, an infectious disease expert at the Harvard T.H. Chan School of Public Health in Boston, Massachusetts, who has modeled social distancing strategies and transmission dynamics of SARS-CoV-2 over the past few weeks.
Researchers use a working range for the virus’ secondary attack rate, which approximates how many people will become sick when in close contact with an infected person — roughly 1 in 3. Modelers also have early numbers for the virus’ incubation period between initial infection and first symptoms (about 5 days, for most people), the time it takes for a COVID-19 infection to run its course (usually 2 weeks), and how long symptomatic people can transmit the virus to others (up to 10 days of showing symptoms, on average).
Continued
These numbers are still estimations. A recent paper out of the University of Oxford suggested that a much larger proportion of the UK has been infected than previously believed, and only a small number of cases require hospitalization. These results are at odds with the more established belief that close to 20% of cases are serious enough to require hospital treatment, as recently reported by the Centers for Disease Control and Infection.
The Known Unknowns
Critically, scientists don’t know for how long people can shed the virus while showing no symptoms, or mild symptoms, themselves. “Practically, that matters a lot,” says Grad. Without knowing when an infected person is contagious, it becomes far more difficult for epidemiologists to figure out where they’ve been and who they’ve been in contact with while carrying the virus, and to estimate the effectiveness of interventions.
As some modelers look months and years into the future, there are several other looming uncertainties. It’s unclear whether SARS-CoV-2 is seasonal, like the flu and other coronaviruses in humans. Researchers also don’t know what role kids play in its spread, nor, crucially, how long immunity will last for people who recover from infection. Antibodies could protect people for life, or they might only offer protection for only a few years. “That continues to be an unknown that will really have big implications for what will happen in the longer term with this virus,” Grad says.
Location Matters
For models that account for state or regional infections, a few factors are important: High population density, levels of public transit, and social gatherings facilitate rapid transmission, as painfully evident in the New York City metro area and New Orleans. “When you’re modeling these things, you have to guess and average how people are interacting with each other,” says Rachel Silverman, PhD, ScM, an epidemiologist at Virginia Tech. “In a place like New York City, riding the subway, you’re exposed to hundreds of people, potentially.”
Communities with larger households and multiple generations mingling under one roof, as is typical in some of the hardest-hit areas of Northern Italy, also quicken the rate of infection. “Italian families tend to be three generations in one household,” says Raymond, of Rutgers University. Finally, the age and health of a population matters for how people will be able to weather disease and the number of hospital resources they’re expected to need.
Continued
The Wild Card
Right now, the biggest unknown we have control over is how much people in the US will respond to shuttered businesses, closed schools, stay-at-home orders, and social pressure to decrease the rate of transmission. “That’s an open question,” says Raymond. “If we all locked ourselves in our houses and didn’t have to ever go out, this would die out much quicker.”
Social distancing regulations vary dramatically across states, and even between counties, and cities. “We almost certainly know the compliance is not the same, and it’s not being applied uniformly,” notes Amanda Simanek, PhD, MPH, an epidemiologist who specializes in the social patterning of infectious disease at the University of Wisconsin, Milwaukee. Scientists are sure, however, that as long as people frequent grocery stores, visit family, and fly across the country, the virus will continue its spread.
Public officials and healthcare workers are trying to get ready for the numbers of patients the models predict. “The last thing we want to have happen is that we’re underprepared for a surge of cases,” says Gregory Schrank, MD, infectious disease specialist at the University of Maryland Medical Center in Baltimore, and one of the leaders of the hospital’s pandemic response team.
Based on all the models Shrank has seen so far, however imperfect and variable by region, the situation remains daunting. “The number of cases and subsequent admissions to the hospital will almost certainly exceed the healthcare capacity of most healthcare facilities,” he says. “Regardless of where they are.”




