What to Know About Newly Approved Alzheimer’s Drug
Jan. 6, 2023 — The highly anticipated Alzheimer’s drug lecanemab was granted accelerated approval status this afternoon by the FDA, offering hope where there has been little for patients and their families affected by the devastating disease.
More than 6 million people in the U.S. live with Alzheimer’s.
It’s not a cure, but the drug, given intravenously every 2 weeks, has shown moderate positive effects in clinical trials in slowing early-stage disease.
But many are wary. As explained in an editorial last month in the journal The Lancet, “The Alzheimer’s disease community has become accustomed to false hope, disappointment, and controversy.”
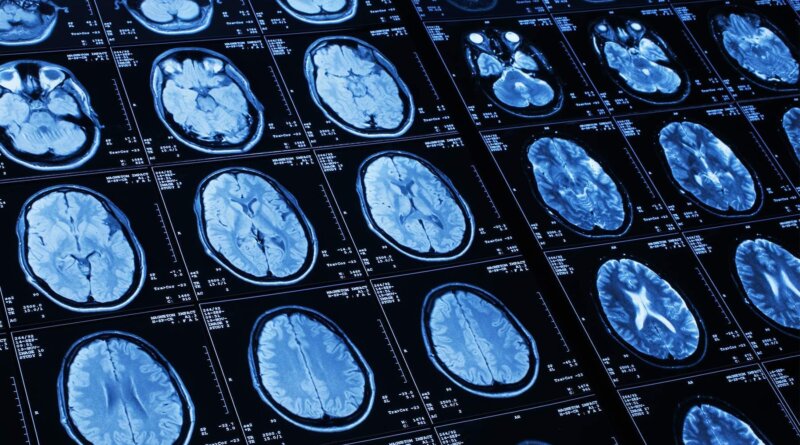
Some worry about lecanemab’s safety as some people in clinical trials experienced serious side effects of bleeding and swelling in the brain. Scientists recently attributed a third death to lecanemab, brand name Leqembi, though the drugmaker disputed the medication was the cause.
So what should patients and their families make of today’s news? Here we answer some of the top questions surrounding the drug.
What Does Today’s FDA Action Mean?
The FDA granted accelerated approval to Leqembi after it showed positive trial results in slowing the progression of early-stage disease.
The FDA can grant accelerated approval for drugs that treat serious conditions and fill an unmet medical need while drugs continue to be studied in larger trials.
With the FDA approval in hand, doctors can now prescribe the medication.
Rebecca Edelmayer, PhD, the Alzheimer’s Association senior director of scientific engagement, says that with the FDA’s move today, ramping up manufacturing — and eventually nationwide distribution and implementation — will take some time.
“Ask your doctor about availability,” she says. “The main issue is that, without insurance and Medicare coverage of this class of treatments, access for those who
could benefit from the newly approved treatment will only be available to those who can pay out-of-pocket. Without coverage, people simply won’t be able to get the treatment.”
The Washington Post reports that with accelerated approval, drugmaker Eisai is expected to immediately apply for full FDA approval, which wouldn’t be likely to come before later this year. Full approval could help clear the path for Medicare coverage of the drug.
Potential Benefit?
Those who got Leqembi in a clinical trial for 18 months experienced 27% less decline in memory and thinking relative to the group who got a placebo. It also reduced amyloid in the brain, the sticky protein that builds up in the brains of people with Alzheimer’s and is considered a hallmark of the disease.
Howard Fillit, MD, co-founder and chief science officer of the Alzheimer’s Drug Discovery Foundation, says, “It’s the first phase III study in our field of a disease-modifying drug where the clinical efficacy was very clear.”
Concerns About Side Effects
The drug has raised safety concerns as it has been linked with certain serious adverse events, including brain swelling and bleeding. In the trial, 14% of patients who received the drug experienced side effects that included brain swelling and bleeding, compared to about 11% in the placebo group.
Scientists have reportedly linked three deaths during the clinical trial to lecanemab, though it is unclear whether it caused the deaths.
Fillit notes that the first two people who died were on blood thinners when they received lecanemab.
“There are things about the use of the drug in the real world that we need to work out, especially in the context of people with comorbidities,” he says.
The third death is a little different, Fillit says. The patient, who had a stroke, showed signs of vasculitis, or inflammation of the blood vessels.
“We don’t know exactly what happened, but we do know it was very, very rare” among the people involved in the trials, he says.
Edelmayer says that the most common reported side effects during the trials were infusion-related reactions, headache, and amyloid-related imaging abnormalities (ARIA). According to the FDA, these abnormalities “are known to occur with antibodies of this class. ARIA usually does not have symptoms, although serious and life-threatening events rarely may occur.”
The FDA has added these as warnings to the drug’s label, describing the possible infusion-related reactions as flu-like symptoms, nausea, vomiting, and changes in blood pressure.
How Much Will It Cost?
Eisai says that lecanemab will cost $26,500 a year.
In a draft report released in December, the Institute for Clinical and Economic Review (ICER) said a price ranging from $8,500 to $20,600 a year would make the drug cost-effective. While the group has no authority to set prices, many large health insurers consider its reports when they negotiate prices and some drugmakers take into account ICER’s recommendations when setting prices.
An editorial in The Lancet last month warns that the cost will likely be “prohibitive” for low- and middle-income countries and many health systems don’t have the infrastructure for a widespread rollout.
Will Medicare Cover it?
The Centers for Medicare and Medicaid Services (CMS), which runs Medicare, which covers most people with Alzheimer’s, has indicated it won’t broadly cover amyloid-lowering drugs until the drug gets full U.S. approval based on clinical benefits, as opposed to accelerated approval.
That means people would have to pay thousands out of pocket at first to get it.
The CMS decision effectively denies Medicare coverage of fast-tracked FDA-approved medications for Alzheimer’s disease unless the person is enrolled in an approved clinical trial.
On Dec. 19, the Alzheimer’s Association filed a formal request asking CMS to remove the trial-only requirement and provide full and unrestricted coverage for FDA-approved Alzheimer’s treatments.
CMS says in a statement after today’s announcement: “Because Eisai’s product, lecanemab, was granted accelerated approval by the FDA, it falls under CMS’s existing national coverage determination. CMS is examining available information and may reconsider its current coverage based on this review.”
“If lecanemab subsequently receives traditional FDA approval, CMS would provide broader coverage,” the statement says.
Who Benefits Most From This Drug?
Lecanemab is a treatment for people with early-stage Alzheimer’s disease who have amyloid in their brain. This means people with other types of dementia, or those in the later stages of Alzheimer’s disease, are not likely to improve with this drug.
Who Makes Lecanemab?
Japan-based Eisai is developing the drug, a monoclonal antibody, in collaboration with the U.S. company Biogen.
What’s the Alzheimer’s Association’s View?
The association urged accelerated FDA approval. In a statement, it says it “welcomes and is further encouraged” by the clinical trial results.
It says data published in the New England Journal of Medicine confirms lecanemab “can meaningfully change the course of the disease for people in the earliest stages of Alzheimer’s disease.”
“We are energized at the progress we are seeing in the research pipeline. The science is telling us that although anti-amyloid treatments are not a cure — they are not going to be the end of
treating Alzheimer’s — they are certainly the beginning,” Edelmayer says.
Are There Alternatives?
The FDA gave accelerated approval to Biogen to produce another drug for Alzheimer’s, Aduhelm (aducanemab), in 2021, but the move was controversial as the drug’s effectiveness was widely questioned. It has since largely been pulled from the market.
Aduhelm had been the first approved early-stage Alzheimer’s treatment since 2003.