Doctors Perform First Surgery on Baby’s Brain in the Womb
May 5, 2023 — In a first-of-its-kind surgery, doctors have successfully repaired a malformation in the brain of a fetus still in the womb.
The team from Boston Children’s Hospital and Brigham and Women’s Hospital used ultrasound guidance to repair the vein of what’s known as a Galen malformation, which causes excessively high blood flow and can lead to neurologic and heart complications, including heart failure, severe brain injury, and death soon after birth.
The surgery was performed on a 34-week fetus with remarkable results. Since birth, the baby girl, who was identified while in the womb as being at high risk of suffering serious complications of the malformation, has required no medication to treat heart failure and no further surgery.
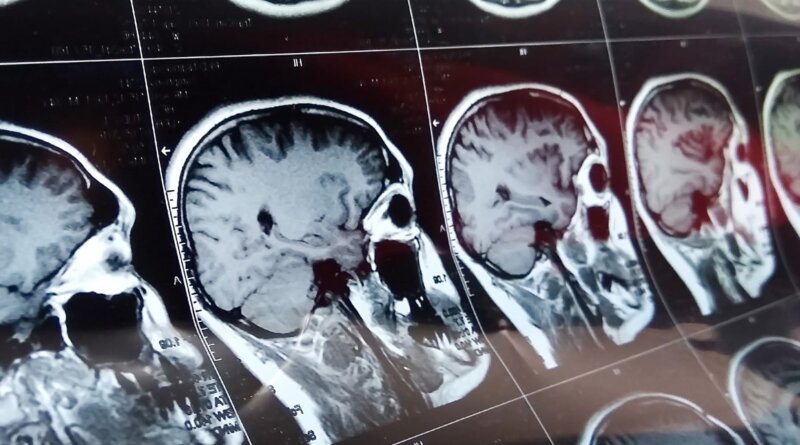
Repeated echocardiograms after the girl’s birth showed marked improvement in heart function, and a brain MRI showed no injury and a normal neurologic exam.
“This is incredibly exciting. The hope is that this baby, and others with this condition who receive this in-utero surgery in the future, will go on to have a normal life,” lead researcher Darren B. Orbach, MD, PhD, said.
“We were thrilled to see that the aggressive decline usually seen after birth simply did not appear,” he said. “We are pleased to report that at 6 weeks, the infant is progressing remarkably well, on no medications, eating normally, gaining weight, and is back home. There are no signs of any negative effects on the brain.”
Vein of Galen Malformation
Orbach said that vein of Galen malformation, which occurs in about 1 in every 60,000 births, is an anomaly where the arteries directly connect to veins rather than to capillaries that are necessary to slow blood flow and deliver oxygen to surrounding brain tissue.
“The arterial and venous systems are fundamentally very different. The arterial system is high pressure, high flow; while the venous system is low pressure, low flow. They shouldn’t be directly connected,” he said.
The vein of Galen malformation is the most extreme version of such an anomaly. Developing early in a baby’s formation, it is known to produce a large increase in blood flow through the brain that grows over time and can sometimes cause the heart to work twice as hard.
The placenta is believed to protect against this, as most babies don’t have physiologic problems in the womb, but they can run into crisis after birth, with the extremely high blood flow causing a major stress to the heart.
Typically, babies develop heart failure as their first major symptom soon after birth, Orbach said. “Although the anatomical problem is in the brain, the clinical manifestation is high-output heart failure. The heart is trying to do double its normal work, pumping the blood to the malformation and immediately back to the heart and that blood is not performing any useful function.
“These newborns can get very sick. They need multiple medications to support their cardiovascular system, and we need to do procedures to try and reduce the blood flow,” he said.
Brain injury is also a common problem. “The brain circulation is very abnormal. The blood is being shunted through the malformation rather than circulating through the brain tissue,” Orbach said.
“The babies who get sick would have a very high mortality (up to 90%) without expert care. Even those who do receive expert care at a specialty center have a mortality rate of 30% to 40%, and those who survive have a high risk of neurologic and cognitive impairment,” he said.
The current treatment for babies born with the condition involves a catheter inserted into the arteries in an attempt to close the malformation.
But Orbach said some babies are born too sick to have the operation. “The heart failure and brain injury is so overwhelming that no matter what we do, we cannot reverse it, and these babies normally do not survive. What we are doing with the fetal surgery is trying to help those babies who cannot be treated with the current postnatal approach,” he said.
Although other fetal surgeries are now routinely performed, this is believed to be the first in-utero surgery aimed at the cerebrovascular system.
“There were a lot of uncertainties,” Orbach said. “We didn’t even know if we would be able to see our instruments on ultrasound.” To model the procedure, the researchers had a phantom fetal skull and brain constructed with a vein of Galen malformation, which was key to obtaining FDA approval for the study.
If the study shows success in the other patients too, the technique could be rolled out to other centers. “There definitely needs to be fetal surgery and neuro-interventional teams familiar with vein of Galen malformation in place, and ready to manage complications after delivery regardless of outcome. But we are not the only center with those capabilities, so if our trial pans out, yes, the hope is that other teams in specialist children’s hospitals around the world could do this too,” he said.