Lap Band Failures Drive Many to Safer Weight Loss Surgeries
March 29, 2022 — Jessica Furby struggled with weight most of her life, constantly dieting and exercising to shed pounds. But nothing seemed to help. By her 22nd birthday, she tipped the scales at more than 300 pounds.
So, in 2011, while a college student in Pittsburgh, she decided to have a weight loss procedure known as lap band surgery. Doctors placed a synthetic belt around her stomach to limit what she could eat. It seemed like a good option at the time and, after her surgery, she lost about 60 pounds.
But the benefits didn’t last. In the months that followed, she had pain and other complications. Worst of all, she eventually regained all the weight she’d lost — and then some. By 2016, she weighed 350 pounds and was becoming prediabetic.
That’s when she decided to have the band removed and, on her doctor’s recommendation, had another procedure — gastric sleeve surgery — where surgeons remove about 80% of the stomach.
Studies have found the sleeve surgeries carry fewer complications and a much higher success rate than lap band procedures, which Furby’s experience has confirmed.
Today, at age 32, she’s down to 288 pounds and says she is on her way to hitting her ultimate goal of 200 pounds.
“The surgery has been a godsend,” she says. “I have not had any complications with it at all. The sleeve was life-changing for me.”
Furby’s experience has become more common as the risks, complications, and failures of lap band surgeries have been rising over the past decade.
More band patients are choosing to have conversion surgery to gastric sleeve and a similar bariatric procedure known as gastric bypass. At the same time, fewer doctors are doing lap band procedures, because of problems like Furby’s.
According to the latest figures from the American Society for Metabolic and Bariatric Surgery, lap band procedures account for fewer than 1% of the 256,000 bariatric operations done in the U.S. each year, while gastric sleeves add up to nearly 60%. That makes sleeve surgeries the most commonly performed bariatric operation today.
By comparison, 35% of bariatric surgeries were lap band procedures in 2011, while sleeve operations accounted for under 18%.
Furby’s surgeon, Anita P. Courcoulas, MD, says the trend is being driven by many of the things Furby experienced firsthand.
Courcoulas, who is chief of minimally invasive bariatric and general surgery at the University of Pittsburgh Medical Center, says there are two main reasons for the decline in lap band procedures.
“It has been shown to be less effective for weight loss [than] other bariatric surgical procedures, and band intolerance often results in band removal,” she says.
Gastric sleeve, followed by gastric bypass, are the two most commonly performed operations in the United States and worldwide, she says.
Courcoulas says the shift from gastric bypass to gastric sleeve procedures “is likely driven by the decline in the band usage, patient preferences for a less invasive operation, such as the sleeve compared to bypass, and surgeon preferences about which operation(s) to offer a given patient.”
Ali Aminian, MD, director of the Bariatric and Metabolic Institute at the Cleveland Clinic, agrees that lap band complications and failures, in addition to ineffective weight loss, are behind the trend, driving patients and doctors to choose safer and more effective procedures.
He says the Cleveland Clinic no longer does band operations, and he has done a lot of conversions.
“Around 50-60% of [lap band] patients require reoperation to take care of the complications,” he says. “So, when you have a surgery where more than half of the time the patients require reoperation, we cannot claim that’s a safe operation.”
Evolution in Bariatric Surgery
The first bariatric surgeries for weight loss date back to the 1950s and 1960s, when surgeons at the University of Minnesota first did experimental bypass operations. Adjustable gastric banding first appeared in the late 1970s and early 1980s.
But these procedures didn’t gain widespread mainstream use until gastric band procedures gained full FDA approval in 2001. Clinical trials have found people who have bariatric surgery have a significantly lower risk of heart disease and other obesity-related health problems.
In the decade that followed the FDA’s approval of lap band surgery, it became a popular weight loss procedure, accounting for more than a third of all bariatric surgeries by 2011.
“Fifteen to 20 years ago, lap band was the most commonly performed procedure for bariatric surgery worldwide and in the United States,” Aminian says. “It was very easy to do, it was quick — it takes 20 minutes to do the procedure — recovery was short, and initially patients had great outcomes. They would lose weight and were healthy.”
But over the past decade, surgeons found that patients often regained the weight they’d lost, and complication and failure rates rose.
“Because the lap band is a foreign body that we place inside the body, many patients had complications related to that foreign body,” Aminian says.
The band can sometimes move or be displaced, causing blockage of the stomach, experts note. Other common complications include nausea, vomiting, acid reflux, and esophageal issues (such as a hard time swallowing). Some patients feel pain, constant food cravings, or that they can’t eat or drink anything. And painful infections and other problems can develop with the tubing or the port placed under the skin that is connected to the band, which doctors use to make adjustments after surgery.
“Scar tissue can also form around the lap band that can cause a blockage in the stomach,” Aminian says. “Then if the band is too tight, it can erode into the stomach tissue or even go inside the stomach and cause perforation or bleeding.”
By contrast, gastric sleeve and bypass procedures have been found to be safer, result in longer-lasting weight loss, carry fewer complications, and require fewer patient reoperations. Aminian estimates that only 2% to 3% of patients need second operations.
Another Key Factor: Metabolic ‘Reset’
Sleeve and bypass procedures also offer another critical advantage over band operations: They help reset the body’s metabolism better, changing appetite- and weight-related hormones in the body.
Those hormones can affect food cravings, help people feel full after eating, or boost weight gain in ways that can trump willpower, experts say.
“The lap band doesn’t change the hormones in the body, it’s just a restrictive band around the esophagus or the upper part of the stomach, so it limits the patient’s ability to eat too much,” Aminian says. “That’s why it doesn’t have the metabolic effects.”
But other procedures, like the gastric sleeve, change the hormones in the body. Removing the source of those hormones means the patient won’t have the same appetitie, Aminian says.
“And that’s why it’s very effective. The problem with the lap band is the patient always has the feeling and desire to eat — they’re always hungry. That’s why in the long run, they fail,” he says.
“They change the setpoints,” Aminian says. “When the hormones in your body change, the [metabolic] setpoint in the brain also changes.”
He likens the metabolic setpoint to a thermostat in your home that regulates temperature inside.
“When a patient goes on a diet or goes on the lap band, the thermostat doesn’t change,” he says. “They may lose some weight, but they’re going to regain it because the thermostat is the same. But when the hormones in your body change, then the thermostat will change and you’re not going to regain the weight that you have lost.”
Sachin Kukreja, MD, a surgeon and CEO at DFW Bariatrics and General Surgery in Dallas, says he believes these metabolic changes are the biggest things behind successful surgeries.
“People synonymize bariatric surgery with weight loss surgery, but really the metrics we should be using are more related to metabolic measures,” says Kukreja, who hasn’t done a band surgery since 2013. “And so, the metabolic parameters that change with bariatric surgery are much more significant in the setting with sleeve and gastric sleeve, and much less significant with lap band.”
David Arterburn, MD, agrees that resetting metabolism is important but says the issue is “controversial and challenging” among bariatric surgeons.
“The metabolic setpoint is the idea that we have a biologically controlled set body weight that we will always return to. Clearly, this is not the case for everyone, as some people lose and maintain long-term weight loss,” says Arterburn, a general internist and bariatric surgery researcher at Kaiser Permanente Washington Health Research Institute.
Post-Op Lifestyle Changes Critical to Success
Bariatric surgeons and patients alike also say that no surgical procedure is a magic-bullet solution for weight loss. Patients who have any type of bariatric surgery must embrace post-op lifestyle changes — eating healthier diets, getting more exercise, cutting out unhealthy habits — to lose weight and maintain weight loss.
Jan Lasecki, 54, a health care specialist in Akron, OH, who had band-to-sleeve conversion surgery in 2020, says the post-op follow-up was at least as important as the surgery itself in helping her shed pounds.
She says at first, she chose lap band surgery several years ago because it was “less invasive” than gastric sleeve or bypass. But while she lost about 50 pounds, she regained it after about 6 years and had other complications.
So, 2 years ago, Lasecki had two surgeries 6 months apart — one to remove her band, and a second to create a gastric sleeve. And the results, she says, have been very successful, in part because of the changes she made after surgery, with the help of her doctor’s staff.
“I have now lost about 90 pounds and have kept if off since surgery,” she says. “I would tell anyone considering any bariatric surgery, it was definitely worth it [and] having the sleeve resulted in greater weight loss.”
The follow-up was key to the success, she says.
The staff “have the tools and support to help you when you tend to fall back on old behaviors and start to regain weight,” Lasecki says. “They can help you before it gets out of control. I had no issues following either procedure from a surgery perspective.”
Sally and Robert Cordova — who had gastric bypass and sleeve surgeries, respectively, 3 years ago — agree that the post-op lifestyle changes are critical to success.
“When we agreed to have this surgery, we agreed that this will be a lifestyle change for the rest of our lives,” says Sally, 48, an accounting specialist who’s lost 150 pounds — half her body weight — since her surgery. “You can’t just get to your ideal weight and then stop.”
Robert, 47, a federal border control agent whose workmates nicknamed him “Big Rob” when he tipped the scales at 336 pounds, says it’s a mistake to think of the surgery as a “magic-bullet” solution to obesity. There’s more to it than that, he says.
“One of the things I like about the process I’ve taken is, in my opinion, they set you up for success,” he says. “Because it’s not just having the surgery and you’re done; it’s all the classes educating you about all the lifestyle changes you have to do, and starting them before the surgery. The only people that I know personally who haven’t been successful with the surgery are those who haven’t made the lifestyle changes.”
Today, at 230 pounds, Robert says he’s never felt better.
“I feel great,” he says. “I have become more active, obviously doing everything is a lot easier. It got to the point where it was a task to just tying up my shoes!”
Should Band Patients Convert to Sleeve or Bypass?
Bariatric surgeons interviewed for this article were reluctant to say that all people who had lap band procedures should convert to gastric sleeve or bypass. But they made it clear that sleeve and bypass procedures are safer and more effective than lap band surgery, which is why it is rarely done today.
“If a patient experiences poor weight loss or complications from a band, they can consider conversion/revision to a sleeve or bypass,” says Courcoulas, echoing the views of other doctors.
“The choice of revision procedure should be based on patient factors, including diabetes and total weight. Converting a band to a sleeve is a technically easier operation, and some studies show that there are fewer complications, compared to conversion to a bypass. These considerations need to be balanced with data that show that both weight loss and metabolic improvements such as diabetes are greater after bypass, compared to sleeve.”
Doctors and experts also say it’s important for patients who are considering a lap band conversion to gastric sleeve or bypass to understand the differences among these three primary procedures, all endorsed by the American Society for Metabolic and Bariatric Surgery.
Here’s a primer, including the pros and cons of each procedure:
Lap Band
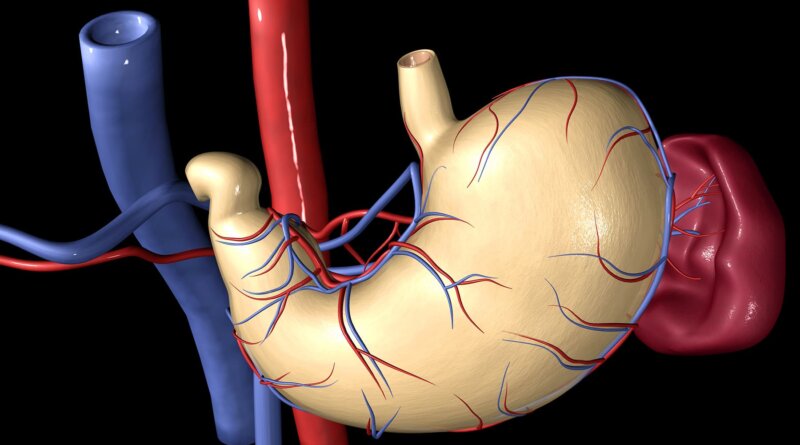
In lap band surgery, an adjustable gastric band made of silicone is placed around the top part of the stomach, creating a small pouch above it, to limit the amount of food a person can eat. The size of the opening between the pouch and the stomach can be adjusted with fluid injections through a port placed underneath the skin.
Food goes through the stomach but is limited by the smaller opening of the band.
Advantages:
- Lowest rate of complications right after surgery
- No division of the stomach or intestines
- Patients go home on the day of surgery, and recovery is quick.
- The band can be removed, if necessary.
Disadvantages:
- The band may need to be adjusted, from time to time, and patients must make monthly office visits during the first year.
- There’s less weight loss than with other surgical procedures.
- It comes with the risk of band movement (slippage) or damage to the stomach over time (erosion).
- The surgery means that a foreign implant has to remain in the body.
- It has a high rate of reoperation.
- The surgery can bring swallowing problems, enlargement of the esophagus, and other complications.
Gastric Sleeve
For laparoscopic sleeve gastrectomy — often called gastric sleeve — surgeons remove about 80% of the stomach, so the remaining stomach is the size and shape of a banana.
The new, smaller stomach holds less food and liquid, reducing how much food (and how many calories) the patient can get. By removing the portion of the stomach that produces hunger and appetite hormones, the surgery also helps reset the body’s metabolism — decreasing hunger, increasing feelings of fullness, and allowing the body to reach and maintain a healthy weight as well as control blood sugar.
Advantages:
- It’s technically simple and has a short surgery time.
- It can be done in certain patients with high-risk medical conditions.
- It may be the first step for patients with severe obesity or as a bridge to gastric bypass.
- The surgery brings effective weight loss and improvement of obesity-related conditions (typically 50%-60%, Mayo Clinic estimates), with a low complication rate (2%-3%).
Disadvantages:
- Nonreversible procedure
- May worsen or cause new reflux and heartburn
- Less impact on metabolism, compared to bypass procedures
Gastric Bypass
Gastric bypass, also known as the Roux-en-Y gastric bypass (French for “in the form of a Y”) is another effective procedure used to treat obesity and obesity-related diseases (done laparoscopically since the 1990s).
For the operation, surgeons divide the stomach into a smaller top portion (pouch) about the size of an egg, then the larger part of the stomach is bypassed and no longer stores or digests food.
The small intestine is also divided and connected to the new egg-sized stomach pouch to allow food to pass.
Gastric bypass works by limiting the amount of food and calories a patient can consume. It also decreases hunger and increases fullness, allowing the patient to reach and maintain a healthy weight. The impact on hormones and metabolic health often results in improvement of diabetes and helps patients with reflux.
Advantages:
- Reliable and long-lasting weight loss
- Effective for remission of obesity-associated conditions
- Effective weight loss (60%-70%, Mayo Clinic estimates)
Disadvantages
- Technically more complex when compared to gastric sleeve or band
- More vitamin and mineral deficiencies than with gastric sleeve or band
- Risk for small bowel complications and obstruction, as well as ulcers, especially with NSAID or tobacco use
- May cause “dumping syndrome,” a feeling of sickness after eating or drinking, especially sweets